Coronary artery disease refers to a condition caused by the coronary arteries being blocked or constricted.
Causes of Coronary Artery Disease
Coronary artery disease is the result of a buildup of plaque around the interior wall of the arteries, causing the lining of the arteries to thicken and become constricted. When this happens, the heart can’t pump as much oxygenated blood as required.
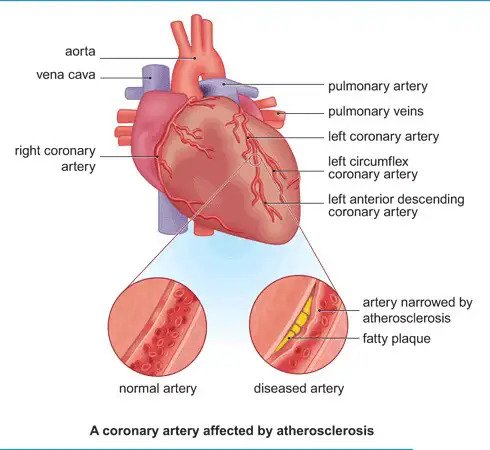
Over time, if a patient develops coronary artery disease, his or her blood vessels will no longer be able to supply sufficient oxygenated blood to the heart muscle, which can lead to sudden and severe chest pains or heart attack.
If there is a sudden blockage of the arteries caused by deposits of plaque, a rupture or a blood clot may then develop, resulting in a potentially fatal heart attack and other serious related complications.
Symptoms which should cause patients to consult their doctor
- A crushing pain in the chest is a typical symptom of coronary heart disease: the pain is severe, and is often likened to a heavy load being placed on top of you, or being squeezed around the chest or underneath the sternum.You may also experience a pain in the neck, jaw, shoulders and arms, especially on your left side, and particularly during exercise, lasting for around 2-3 minutes. When seated, or when taking medication to dilute the blood vessels under the tongue (also known as nitrates), the symptoms should improve.
- Easily tired during physical activity or when exercising. This can take place suddenly and severely in 1-2 weeks, or it can be a chronic symptom lasting for 3 weeks or more.
- Fatigue, shortness of breath, difficulty lying on one’s side, tightness in the chest, shallow breathing and also a crushing chest pain. These symptoms may appear suddenly or periodically and may last for a long time.
- Fainting, as well as tightness of the chest, which is caused by sudden or severe low blood pressure.
- Unconsciousness or cardiac arrest.
How are we using stem cells to understand and treat heart function and disease?
Researchers are using stem cells in two important ways to improve cardiac health.
First, they are turning stem cells into “heart muscle in a dish.” If patients have genetic causes of heart disease, their stem cell-derived heart muscle also will have this disease and this heart muscle can be used to discover new drugs.
ดังนั้นจึงสามารถนำเซลล์กล้ามเนื้อหัวใจนี้ไปใช้ประโยชน์เพื่อคิดค้นตัวยาชนิดใหม่ได้อีกหลายชนิด
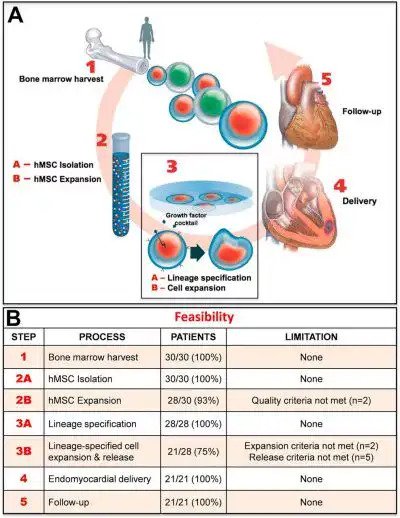
Second, stem cells offer ways to replace damaged heart tissue. Using cellular therapy, researchers hope to repair or replace heart tissue damaged by congestive heart failure and heart attacks.
Unlike the treatments listed above, cellular therapy could provide a durable treatment for heart deficiencies, rather than symptom-focused treatment.
Your heart is constructed of several types of cells. For mending damaged heart tissue, researchers generally focus on three specific heart cell types:
- Cardiomyocytes, the beating muscle cells that make up the atria, the chambers where blood enters the heart, and the ventricles, where blood is pumped out of your heart. Cardiomyocytes are currently being targeted in cellular therapies for heart disease.
- Cardiac pacemaker cells, which send and receive electrical signals to keep your heart beating in rhythm.
- Endothelial cells, which line blood vessels and help deliver oxygen to the cardiomyocytes.

Researchers are experimenting with a variety of stem cell therapies to transplant new cells, use tissue engineering to improve the survival or function of transplanted cells, and stimulate existing cells to generate new cardiomyocytes.
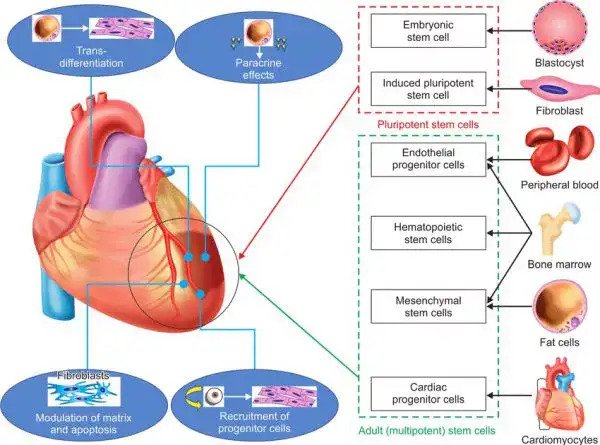
Researchers can grow cardiomyocytes in the lab from the following sources:
- Embryonic stem (ES) cells, cells derived from embryos that can give rise to all cells in the body.
- Induced pluripotent stem (iPS) cells, adult tissue-specific cells that are reprogrammed in the lab to behave like embryonic stem cells and which have the capacity to become any cell type in the body, including cardiomyocytes.
Strikingly, these stem cell-derived cardiomyocytes will beat in unison in a culture dish, the same way they do in a living heart muscle.
This property is essential, as researchers explore whether they might someday grow replacement tissue for transplantation into patients.
However, it is not yet known whether lab-grown cardiomyocytes will integrate or beat in unison with surrounding cells if they are transplanted into a beating human heart.

Cardiac cells made from iPS cells are also incredibly useful for creating human models of heart disease to better understand exactly what goes wrong and for testing different drugs or other treatments. They can also be used to help predict which patients might have toxic cardiac side effects from drugs for other diseases such as cancer.
